

Abstract
Background:
Hypothermia remains an important contributory factor to the mortality of trauma patients in both military and civilian environments. Systems used to mitigate hypothermia in the prehospital environment must strike a balance between weight:size ratio and performance.
Methods:
This study compared the efficacy of three hypothermia mitigation systems; two leading products and the novel Xtract™SR Heatsaver. Mild hypothermia was induced in seven healthy subjects that were rewarmed using these systems. Recordings of aural temperature and a numerical perceived comfort score were made regularly to assess rate of rewarming and perception of the process.
Results:
On all three days subjects placed in the the Xtract™SR Heatsaver recovered from their hypothermic state faster than those placed in the other systems. Clinical assessment could be more easily performed on a patient placed in the Xtract™SR Heatsaver system.
Conclusion/discussion:
Results demonstrate that the new Xtract™SR Heatsaver system offers improved performance with regards to reducing heat loss, increasing patient comfort and allowing for clinical assessment. The study also reinforces the importance of the use of adjuncts such as heat cell blankets and insulation mats alongside hypothermia mitigation systems and provides scope for future research into individual nuances surrounding the effects and onset of hypothermia.
Introduction & background
Accidental hypothermia is often defined in contemporary literature as body temperature below 35°C¹, and remains an important contributory factor to mortality in trauma, both in civilian and military environments². Furthermore, even at 36°C, mortality of severely injured people has been shown to be 11% in civilian and 12% in military patients² . Healthy individuals may experience mild hypothermia as a transient and simply unpleasant phenomenon³, yet for patients with traumatic injuries, hypothermia contributes to a much more significant pathophysiology⁴.
Patients enter a hypothermic state when their core body temperature falls below the normal physiological parameters and the hypothalamus detects a change in temperature, initiating a feedback loop that increases skeletal muscle activity, thus generating heat¹. This occurs via compensatory mechanisms, such as peripheral vasoconstriction and shivering⁵. The thermoregulatory mechanisms begin to fail as core temperature decreases further, resulting in the pathological effects of hypothermia: fatigue, bradycardia, arrhythmias and eventually asystole⁶.
Hypothermia is widely recognised alongside acidosis and coagulopathy as a component of ‘the lethal triad’ that results in poor outcomes for trauma patients⁷. The exact mechanisms of the impact of low body temperatures in coagulation is not understood and remains an area for further research.
However, current literature suggests hypothermia exacerbates the derangement of clotting pathways⁸. This is especially significant in the context of trauma where 40% of all deaths directly result from haemorrhage⁴. Traditionally, trauma management focuses on the treatment of acute haemorrhage, such as haemostasis through mechanical compression or antifibrinolytic drugs, such as Tranexamic Acid⁸. However, a heightened understanding of the lethal triad promotes the need to clinically address additional factors that result in trauma mortality to significantly improve patient outcomes. Previous research has shown increased survival rates for trauma patients in whom preventative measures were taken prior to the initiation of the downwards spiral of coagulopathy and haemorrhage triggered by the lethal triad⁹ . This study focuses on methods to prevent and reverse hypothermia in critically unwell patients with the aim of diminishing the effects of this component of the lethal triad.
To effectively combat heat loss and minimise the hypothermic element of the lethal triad cycle requires an understanding of the most significant mechanism of heat loss that occur in both healthy individuals and seriously injured people. People lose heat in four ways - conduction, convection, evaporation and radiation¹⁰. It is evident that an injured individual wearing wet clothes, lying on the cold ground, and exposed to the environment, would lose heat via all four mechanisms.
It is widely reported that radiation normally accounts for 50-70% of heat loss in normothermic individuals¹⁰. This data has formed the basis of the use of foil blanket systems in the effort to prevent heat loss from casualties.
The efficacy of such systems relies on the assumption that trauma patients have the same thermoregulatory responses as any healthy member of the population. However, recent research disproves this; as from the time of injury, trauma alters the normal central thermoregulation¹¹ Hypovolemia and the resultant peripheral vascular shut-down results in cold and damp skin that is closer to ambient temperature than that of a healthy individual. Heat loss from radiation in skin at an ambient temperature has been shown to be minimal¹² and so other mechanisms of heat loss; conduction, evaporation and convection, become the focus for the prevention of hypothermia. This study will investigate options for use in the field that has been designed to combat heat loss via these processes.
A further challenge is faced when considering the use of hypothermia mitigation systems in the prehospital environment. The volume, shape and weight of a product allow its transportation and deployment in the field¹³. Where size and weight are not an issue, equipment that actively generates heat using power from the mains or generators are preferable¹⁴. Such systems have proved particularly successful in the operative and post-operative settings by using forced air-warming to promote uniform temperature increases and prolonged thermoregulation in hypothermic patients. However, due to size and reliance on electricity, this equipment is not a viable option for personnel working in prehospital fields such as military and disaster rescue¹³.
Those providing medical care in the austere environment have had to reach a compromise between size:weight ratio, practicality, and efficacy of their rewarming equipment.
Many passive insulation systems on the market are too large and heavy to be transported by those undertaking expeditions to remote areas where vehicular assistance cannot be facilitated¹³. There are, however, some lightweight hypothermia management systems that are used by both military and civilian rescue teams¹³. The first insulation blanket compared with the Xtract™SR Heatsaver, a multi-layered reflective material (Product 1) weighs 1.9kg and comes vacuum packed to reduce its size¹⁵. The other (Product 2), made of 4-ply composite fabric, is an even lighter weight option with a mass of 1.58kg¹⁶. Both systems can be easily carried on expeditions and are widely used, yet they primarily focus on loss of heat by radiation and so may not be optimal in the management of trauma patients experiencing a large haemorrhage. This study focused on comparing these two systems with a new product: The Xtract™SR Heatsaver. This novel approach to a hypothermia mitigation system aims to provide optimal performance in the management of a hypothermic patient while remaining within a size:weight ratio acceptable to pre-hospital clinicians and medical care providers.
Aims, materials and methods
For this study a total of seven normothermic healthy subjects were cooled and then rewarmed on three separate occasions, with the aim of demonstrating both the numerical decrease in the subjects’ core temperature, and subjective qualitative findings regarding comfort. The subjects were also invited to share their experience of both the cooling and rewarming stages. Three different heating systems were utilised in the rewarming stage of the trial, to investigate the performance of Xtract™SR Heatsaver in the rewarming of trauma patients when compared with systems currently used in austere environments.
Subjects
Seven subjects volunteered to participate in this initial trial (Fig. 1). This trial additionally aimed to identify areas for further research through the heterogeneity of subjects, as this highlighted differences that might warrant future investigation.

Location
Subjects were exposed to an environment of 0°C (+/- 1 degree) in a temperature-controlled cold room with a plastic and sediment flooring that imitated an artic setting. Researchers ensured they made minimal entries and exits from the room in order to maintain the temperature of the cold room throughout the investigation.
Clothing
All subjects wore lightweight sports shorts, t-shirts, underwear, and shoes, and were soaked in water using a cold shower prior to entering the room. The clothes were identical on all days to minimise confounding factors.

Systems tested

Measurements and recording materials
Aural temperatures were taken (using a Braun Thermoscan tympanic thermometer) from the subjects and recorded by a team of researchers approximately every 20 minutes. At the same time as this recording was made subjects were asked to give a rating of their perceived comfort on a 1-10 scale. Additionally, a thermal imaging camera was directed at the subjects to demonstrate areas of heat loss throughout the investigation.
Methodology
All three days followed the same conceptual methodology. Once the volunteers had an aural temperature reading of 35°C (+/- 0.5°C) they were placed into different hypothermia systems and the rewarming effects of each system was monitored over time. Heat cells were added to aid rewarming. Heat cells were configured around the abdomen and axillary region in the use of Product 2 and the Xtract™SR Heatsaver. In Product 1, the heat cells were placed only in the locations permitted by the product’s design. Due to the size constraints of the cold room and the limited space for both subjects and those collecting data, different systems were tested and compared on each day of the trial.
On days one and two, respectively, Product 1 and Product 2 were compared with the Xtract™SR Heatsaver. On day three a further investigation was carried out on both Product 1 and the Xtract™SR Heatsaver to assess the practicality of carrying out a suitable and comprehensive clinical assessment in the cold austere environment. The assessments were undertaken in the cold room by an emergency medicine consultant with extensive experience of pre-hospital care in both military and civilian environments.
The clinician wore clothing appropriate for artic conditions, including mitts, to ensure the assessment carried out reflected those challenges faces by medics in cold pre-hospital environments. Each system was reviewed by the clinician against a set of predetermined criteria. These included the ability to communicate with the subject, as well as access to lower limbs, chest, and the antecubital fossa. Access to each area corresponded with the necessity to carry out clinical interventions such as tourniquet placement, chest examination and venous access respectively. The clinician’s experiences were recorded as qualitative data and provide a comparison of the two systems’ clinical functionality.
Results & discussions by day
Day one results

Day one discussion
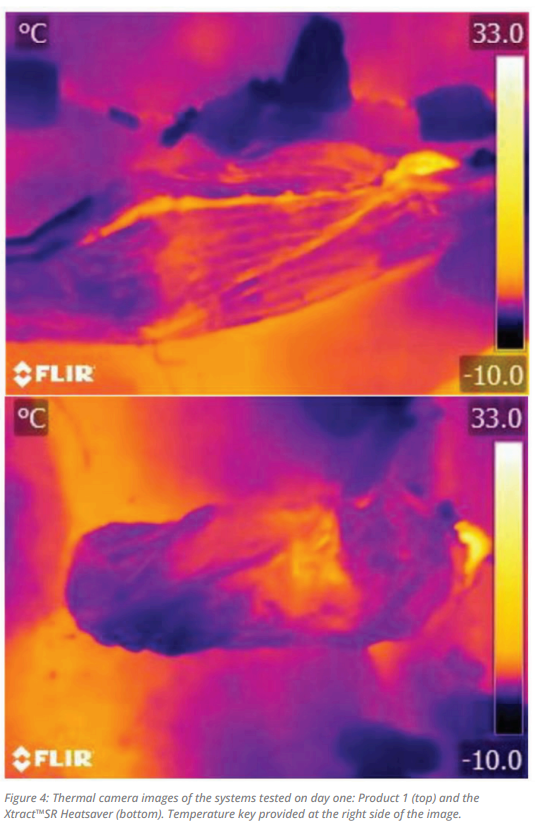
The subject placed in Product 1 struggled to resolve their hypothermic state and their temperature only increased after the placement of a 4mm closed cell foam insulating mat underneath the subject. This was mirrored in the subject’s comfort score which remained below five from the initial hypothermic state until the insertion of the insulating mat. The thermal imaging camera showed heat escaping throughout the system. Conversely temperatures and comfort scores rose immediately when subjects were placed in the Xtract™SR Heatsaver system and thermal imaging camera show reduced heat loss around the core in comparison with Product 1. Interestingly, however, there was a significant area of heat loss around the lower legs when in the Xtract™SR Heatsaver.
Placing an insulated surface under the hypothermic subjects made an immediate positive difference reflected by a rise in both aural temperatures and objective comfort scores. Additionally, targeting core body areas with heat cells and increased insulation increased core temperatures. There was no correlation between heat loss from the legs and decreased temperature or perceived comfort.
The combination of components in the Xtract™SR Heatsaver system addressing conduction, convection, and evaporation as causes of heat loss seem to provide a solution with an acceptable size and weight for medical personnel working in an austere environment.
Day two results

Day two discussion
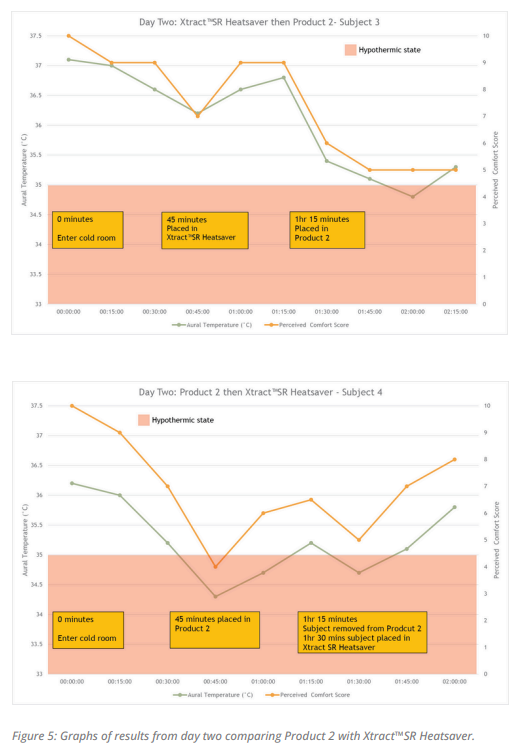
On day two the prototype of Xtract™SR Heatsaver was assessed and compared with Product 2, a product widely utilised by the United States Armed Forces. Consistent with findings from Product 1 on day one this system did not perform well without the provision of additional insulation from the ground. Furthermore, Product 2 relies on the reflection of radiated heat, which, as noted earlier in this paper, is likely not a significant mechanism of heat loss in hypovolaemic patients.
In concordance with day one heat cells were warmed prior to entering the room and were assessed prior to placement to ensure optimum heat production activity during this stage of the trial. Product 2 uses an active heating blanket consisting of 8 cells that are draped over the anterior of the body. Xtract ™SR Heatsaver used a smaller configuration of 4 cells wrapped around the anterior abdomen, extending posteriorly to the kidneys alongside one cell in each axilla. The study on day two further highlighted the importance of combining products that combat all causes of heat loss in an effective, lightweight product of minimal size. Targeting the core with passive and active rewarming mechanisms produced good results and ensures that the Xtract™SR Heatsaver remains within the acceptable size and weight parameter for use in an austere environment.
Subject four was placed in Product 2 and struggled to recover from a hypothermic state. Significant shivering was noted which may explain the initial minor recovery. Due to the clinical status of hypothermia and immediate clinical concerns, a decision was made to move this volunteer into Xtract™SR Heatsaver, where an improvement was seen in core body temperature.
Interestingly the graphical data gathered suggests this improvement took some time. However, it is likely that the 5-minute lag in response of subject’s aural temperature was due to the timings that the aural temperatures were taken, and the time required to move subjects between systems. In contrast to this subject three recovered well inside the Xtract™SR Heatsaver and was moved into Product 2. Once transferred to Product 2 this volunteer’s temperature and comfort scores deteriorated. It can be noted that subject three did not reach a core body temperature of <36°C in the initial cooling phase. This was because subject four cooled quickly but both subjects had to be moved into their hypothermia mitigation systems at the same time to allow the systems to be swapped later in the trial. If an additional Xtract™SR Heatsaver had been available for subject four to be moved into subject three would have been allowed to cool to a more hypothermic state.
Day three results



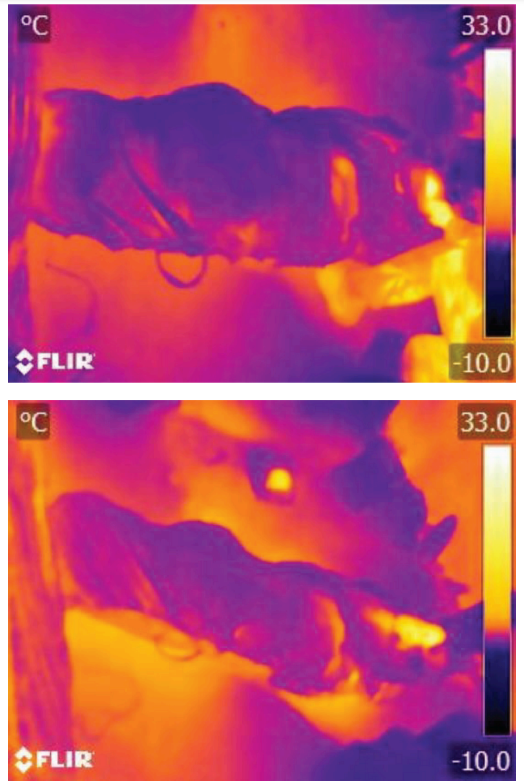
Figure 8: Thermal camera images of the systems tested on day three: Product 1(top), Xtract™SR Heatsaver washed (middle) and Xtract™SR Heatsaver unwashed (bottom).
Day three discussion
On day three the prototype of Xtract™SR Heatsaver was assessed against Product 1 and a washed Xtract™SR Heatsaver. Due to high outdoor temperatures of 32°C and the inability to get the cold room to a temperature below 0°C there was a concern that the subjects may take a long time to reach a temperature of <35°C. A decision was made to move subjects into the hypothermia mitigation systems at 30 minutes as it was agreed that the rate of rewarming could still be compared even with the alteration to the original method set out for use throughout the trial days.
As per previous days heat cells were warmed prior to entering the room and were assessed to be fully active on starting the experiment. Xtract™SR Heatsaver used a smaller configuration of four cells wrapped around the abdomen and extending to the flanks bilaterally alongside one cell under each axilla. Heat cells in Product 1 did not increase the subjects perceived comfort score, perhaps due to their preplacement within the product that resulted in positioning around the cephalic rather than abdominal region.
The washed Xtract™SR Heatsaver system performed to a similar standard as the unwashed prototype suggesting that washing the product did not affect the products insulation capacity. This preliminary evidence may highlight the reusability of this system (unless of course contaminated) and could help prehospital teams to practice within the realms of sustainability and infection control.
For the first time functionality of the products was tested to ensure clinical assessment of the subject was achievable. Xtract™SR Heatsaver performed well with successful completion of the tasks required. Additionally, its openings on both sides allowed easy access for repositioning of the subject without compromising rewarming or exacerbating further injuries through misalignment of the spine.
The main issue with the Product 1 system were practical difficulties associated with communication with patients and opening the Velcro seal to allow examination with mitts on. It was determined that Product 1 performed poorly in this trial as the clinician was required to remove mitts to access the subject for assessment.
General discussion
The subjects’ reports and observations provided an insight into many aspects of cooling, thus highlighting scope for further research into the nuanced mechanisms of hypothermia. As the subjects’ core temperature decreased, they developed cutis anserine, fatigue, intermittent and subsequently, constant shivering⁵. Subjects perceived their feet to be the coldest body area throughout the experiment. However, there was no clinical correlation between perception of foot temperatures and individual core temperatures. It is widely accepted that there is a range of temperatures that can be considered normothermic⁶, what remains to be proven is any correlation between an individual’s normothermic temperature within that range and the rate of cooling. Temperatures for all subjects at the start of the process were within normal physiological range. Interestingly, subject two on day one (a 24-year-old female) started with a lower normothermic temperature and cooled at a slower rate in comparison to the older male subjects. This may be an incidental anomaly but there is scope to incorporate investigation of the impact of age, sex and BMI on the rate of cooling in future trials.
Carrying out each individual investigation highlighted important considerations such as the practicalities of using heat cells within hypothermia mitigation systems and factors relating to the practical deployment of each system. The research highlighted the difficulty of transferring seriously injured patients into a bag like system with only one opening and undertaking clinical tasks while in a cold environment.
Conclusions of the study
The trial improved knowledge regarding the use of active rewarming equipment in the field. It found that the Xtract™SR Heatsaver provided a higher level of comfort and a more immediate relief from hypothermia than other systems currently in use pre-hospitally. Additionally, it was found that heat cells are most effective when pre-warmed in a warm environment and placed over the abdomen and axilla. With further investigation this could change best practice in the pre-hospital environment.
Finally, the investigation resulted in several findings that would support further research²⁰ regarding the mechanisms of hypothermia. It is possible that individual factors such as sex, age and BMI may affect the process of heat loss. Qualitative data showed a decrease in comfort and mood of subjects as temperature dropped. An interesting phenomenon was the initial increased baseline comfort level on the second day of the trial. This could be attributed to the anticipation of the decrease of comfort, adding reserve to the initial comfort rating.

Conclusion on experiment findings and product design
Medical personnel that work in an austere environment are usually limited by the size and weight of the equipment they can select. The ability to avoid or reverse hypothermia is critical in the seriously injured person as its presence comprises a third of the “lethal triad” which becomes a factor to address when aiming to improve survival of trauma patients⁷ . The provision of an effective piece of equipment of an acceptable size:weight ratio will be an integral addition to any critical medical equipment inventory¹³.
The lightweight and small-sized equipment presently available provides some protection from the elements and uses silver foil to reflect radiated heat, known to be the least significant method of heat loss in patients following traumatic injury. These products are minimally insulated and moreover there is no standardised protocol for the use of an insulation mattress¹³ . This study has indicated that present systems do not perform effectively without the addition of an insulated mattress.
The Xtract™SR Heatsaver is slightly larger in size than the other available systems however, it includes an insultation layer that can be placed underneath the casualty. An additional benefit of the Xtract™SR Heatsaver is the Xtract™SR Deployer that stores the components of the product when not in use. This system allows the product to be used in an organised and secure manner while compressing the products to minimise overall size.This research indicated that the Xtract™SR Heatsaver, a product of likely acceptable size:weight, performed strongly in the reduction of all manners of heat loss in the hypothermic individual. The product also proved to be of a practical design that allows medical personnel to easily carry out essential clinical examinations. This product meets the criteria for use in austere environments as an effective treatment of a hypothermic casualty.
Limitations
This research was limited by the small cohort of subjects that volunteered to trial the rewarming systems. It was sensible to use a small sample size in this preliminary trial as it took place in a location that was limited by size. Furthermore, the researchers at this early stage only had access to a few prototypes of each system. Future trials will benefit from a larger cohort which will increase representation in the variables of sex, age and BMI to ascertain any potential influence of these factors on the rewarming process. Future trials would benefit from extending over a longer period, with a larger cohort and in an environment that better controlled cofounding factors such as subject’s diet and sleep prior to the study. Additionally, an element of blinding for both the subjects and the researchers working in the environment may be difficult to achieve but would remove both confirmation and acquiescence bias.
Conflicts of interest
Participating researchers contributed to the design of the Xtract™SR Heatsaver. Independent researchers were present to oversee the deployment of the equipment and data collection to minimise any elements of vested interest. Two of the volunteer subjects were involved in writing up this report.
Download our 'Hypothermia management, an evaluation of a novel lightweight system' by using the form below!

References
1. Bennet B et al. Management of Hypothermia in Tactical Combat Casualty Care: TCCC Guideline Proposed Change 20-01. June 2020
2. Wade CE, Salinas J, Eastridge BJ, McManus JG, Holcomb JB. Admission hypoOr hyperthermia and survival after trauma in civilian and military environments. Int J Emerg Med. 2011 Dec;4(1).
3. Petronea P, C Marinib C, Miller I, Brathwaiteat C, Howell R etc al. Factors associated with severity of accidental hypothermia: A cohort retrospective multiinstitutional study. Annals of Medicine and Surgery. 2020 May Volume 55 p.81- 86
4. Curry N, Hopewell S, Dorée C, Hyde C, Brohi K, Stanworth S. The acute management of trauma hemorrhage: A systematic review of randomized controlled trials. Crit Care. 2011 Mar 9;15(2).
5. Hanania NA, Zimmerman JL. Accidental hypothermia. Crit Care Clin. 1999;15(2):235– 249.
6. Epstein E, Anna K. Accidental hypothermia. Vol. 332, British Medical Journal. 2006. p. 706–9.
7. Gerecht R. The lethal triad. Hypothermia, acidosis & coagulopathy create a deadly cycle for trauma patients. Vol. 39, JEMS : a journal of emergency medical services. 2014. p. 56–60.
8. Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, et al. The CRASH-2 trial: A randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess (Rockv). 2013;17(10):1–80.
9. Husum H, Olsen T, Murad M, Heng Y Van, Wisborg T, Gilbert M. Preventing postinjury hypothermia during prolonged prehospital evacuation. Prehosp Disaster Med. 2002;17(1):23–6.
10. Daniel I. Sessler, M.D.; Michael M. Todd. Perioperative Heat Balance. Anesthesiology February 2000, Vol. 92, 578
11. Hypothermia in the trauma patient. B Tsuei, P Kearney. Injury, Int. J. Care Injured (2004)35, 715.
12. Tipton M, Golden F. Essentials of Sea Survival 1, s.l. : Human Kinetics, Inc, 2013.
13. Dutta R. A Comparison of Five Different Hypothermia Enclosure Systems in a Cold Environment. University of Minnesota 2017.
14. 3M Medical. Degrees make a difference- 3M™ Bair Hugger™ Warming Blanket System. 2016. Available from https://multimedia.3m.com/mws/media/1282930O/3m-bair-huggerblanketwarming-system-brochure.pdf. Last Accessed 17/11/2020.
15. Blizzard X A Persys Company. Layer Casualty Trauma Blanket + Heat Pads – XL. Available from: https://www.blizzardsurvival.com/shop/blizzard-3-layercasualtytrauma-blanket-heat-pads/. Last Accessed 20/11/2020.
16. Prometheus Medical. HPMK® - Hypothermia Prevention & Management Kit. Available from: https://www.prometheusmedical.co.uk/equipment/hypothermiapreventionmanagement/hpmk-hypothermia-prevention-management-kit. Last Accessed 20/11/2020.









