

07/05/2024
Unlocking the Intricacies: how do hospitals evacuate patients?
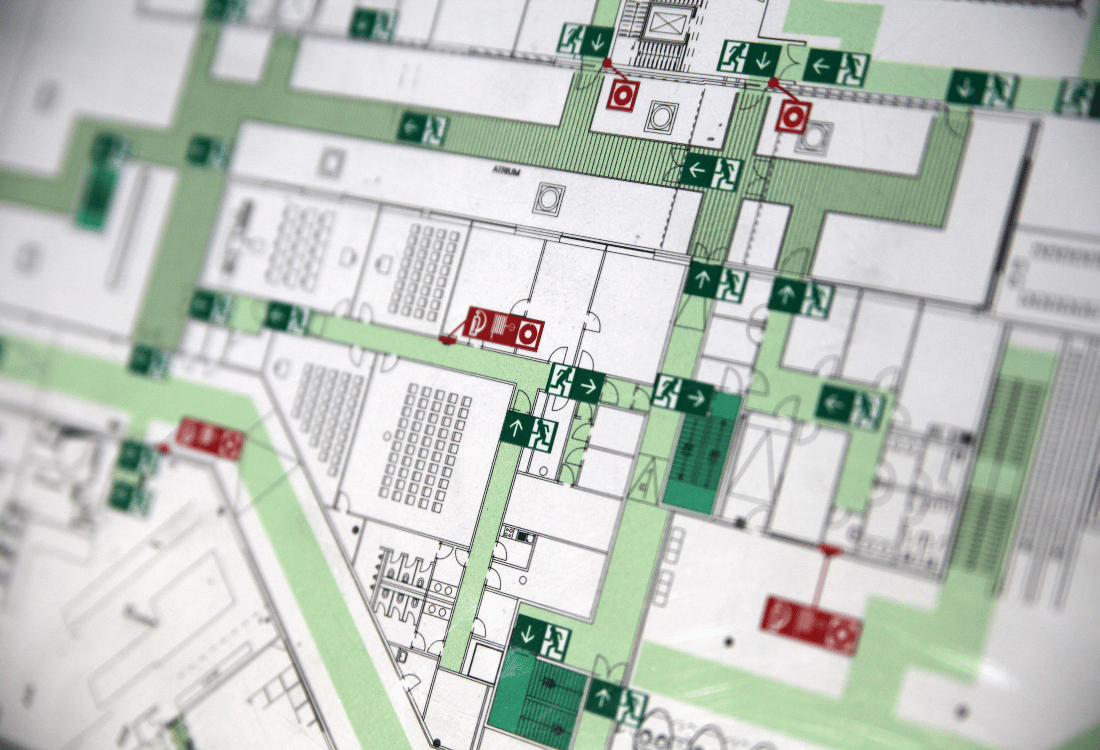
Partial hospital evacuations are more common than many of us realise and whilst full hospital evacuations remain relatively rare, we still need to plan for both. Whether partial or full, hospital evacuations are inherently complex events requiring the moving of multiple ill patients, equipment, staff and supplies whilst maintaining an optimal level of care.
The evidence shows there are several causes, and it depends on where and how they present as to what decisions are made and what the response will be. In some instances, there will be an immediate threat to life requiring a rapid response, in others a more measured approach is possible. Whatever the cause and scale, they can occur at any time and with little prior warning.
Any Evacuation Plan will be activated alongside a Critical or Major Incident Plan. There are key initial decisions that need to be made early on by the Incident Commander, which will then need to be communicated to both internal departments and external agencies. These decisions are fundamental for the response.
1. Level of Evacuation
Depending on number, speciality and location of departments affected, the options are vertical, horizontal, shelter in situ, off-site or a combination of the aforementioned.
2. Evacuation model
How the evacuation is conducted by prioritising geographical layout, availability of resources or acuity of patients.
3. Evacuation Timeline
This depends on the urgency, threat level and time available to prepare patients.
- Immediate threat to life – no preparation time, evacuate immediately.
- Urgent – limited preparation time (1-2 hours) all affected areas 6 hours.
- Planned – extended preparation time e.g. move to new site, potentially over days.
- Prepare – prepare patients only, evacuation may not be necessary.
4. Patient Prioritisation
Key factors are, the resources available, geography and immediacy of the evacuation which varies from hospital to hospital, no two events are the same. A general framework is as follows:
- Those in immediate danger.
- Ambulatory patients.
- Patients who require minimal assistance.
- ITU patients.
5. Evacuation Zones
These are (predesignated) areas of safety that can be activated to temporarily accommodate patients until a ward, that meets their care requirements, can be identified. There could be multiple evacuation zones activated depending on the scale of the event and patient profiles affected. It may also include accelerated discharge for those patients applicable.
6. Staffing Reception Point
Evacuations as well as complex, are extremely labour intensive. Off duty staff maybe called in to assist with the response. The staffing reception point is where they should report to and be allocated duties or tasks.
These decisions dictate the initial response, however an Evacuation Plan should remain flexible, as situations can change rapidly whether it is the cause, its resolution, the hospital’s capabilities or patients’ profiles.
From the embryo stage of an event, communication with clear, accurate information and standardised terminology, is fundamental to driving decision making. As such, and given the nature of an emergency situation, lines or channels of communication should be kept to a minimum, to allow the passage of critical information upstream and downstream, internally and externally.
To find out whether your hospital’s evacuation plan is up to scratch, please book a free hospital evacuation consultation with the team at TSG Associates today.
Image Source: Canva











